The thyroid gland is a butterfly shaped gland located in the low neck straddling the trachea (windpipe). We refer to the two wings of the butterfly as the right and left lobes and the small middle connecting portion as the isthmus. The thyroid gland part of the endocrine system producing thyroid hormone which controls the overall metabolism (speed) of the body.
 Thyroid Disorders
Thyroid DisordersThere are two main categories of thyroid disorders that are mostly separate issues. First, the thyroid can produce too little or too much thyroid hormone which is measured by a blood test. Secondly, the thyroid gland can be enlarged (goiter) or lumpy (nodules) which is best evaluated by ultrasound imaging.
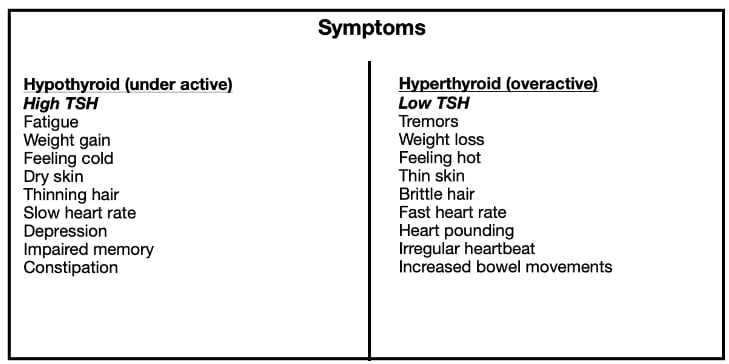
Thyroid glands commonly malfunction and don’t produce enough thyroid hormone (underactive = hypothyroid). The vast majority of these are caused by an inflammation of the thyroid gland called Hashimoto’s thyroiditis. Less common is a thyroid gland where the body produces too much thyroid hormone (overactive = hyperthyroid). The most common cause is Grave’s disease. Hypothyroidism is easily treated by taking a daily pill of thyroid hormone replacement, most commonly levothyroxine. Hyperthyroidism can be treated with medications such as methimazole or propylthiouracil (PTU), radioactive iodine (RAI) or surgery to remove the overactive thyroid gland. Hashimoto’s and Grave’s disease are both autoimmune disorders where your body’s own immune system defectively attacks your thyroid gland causing it to produce an incorrect amount of thyroid hormone. A blood test measuring your TSH (Thyroid Stimulating Hormone) is the way to determine if the thyroid gland is functioning normally. Normal reference ranges vary slightly with each lab but a normal TSH range is generally 0.5 to 5. Because the hormones in the endocrine system work based on a negative feedback loop, a high TSH would indicate hypothyroidism (underactive) and a low TSH would indicate hyperthyroidism (high TSH).
The second category of thyroid disorders relates to size of the thyroid gland and lumps within it. Sometimes the entire thyroid gland become enlarged (goiter) and commonly the thyroid gland will have lumps (nodules) for unknown reasons. This is best determined by thyroid ultrasound. Sometimes numerous lumps in the thyroid gland cause the entire gland to be enlarged (multinodular goiter). An enlarged thyroid gland (goiter) sometimes requires surgical removal because it is too large pushing on nearby structures such as the esophagus (swallowing) and the trachea (windpipe for breathing). Large goiters can grow down into the chest (substernal goiter) or outward causing the neck to look big.
It is estimated that approximately 5-10% of the population has a thyroid nodule that can be felt on exam, and between 30-85% have tiny thyroid nodules that are too small to feel. In most people with thyroid nodules and goiters, the gland produces a normal level of thyroid hormone (euthyroid state). Statistically, approximately 5-10% of nodules are cancerous. Some patients have findings that increase the risk of malignancy. A history of exposure to ionizing radiation (x-rays, nuclear plants) to the neck is such a risk factor, as is a family history of thyroid cancer. Hoarseness and lymph node enlargement can also increase the risk of malignancy. Fortunately, the vast majority of thyroid cancers are treatable and carry an excellent prognosis.
Thyroid ultrasound gives lots of information about the thyroid nodule such as the features of the thyroid gland. Some ultrasound findings are more likely to be benign (not cancer) such as spongiform or cystic (fluid-filled nodule) while other features are more worrisome for malignancy (cancer) such as irregular margins or micro-calcifications. The features seen on ultrasound are rated on a TIRADS scale of one to five, with one being good and five more worrisome. The TIRADS score combined with the size of the nodule determines (based on 2015 American Thyroid Association guidelines) whether we advise observation vs. Fine needle biopsy (FNA).
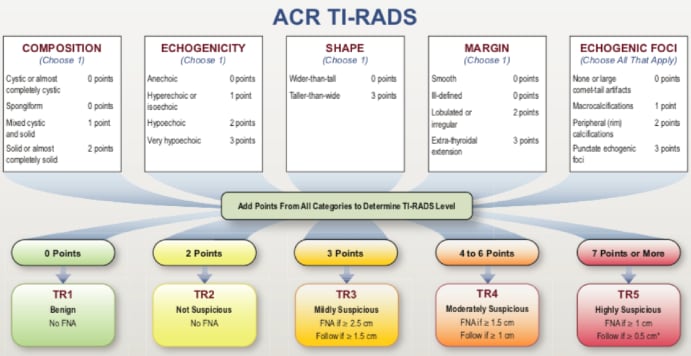
FNA is most reliably done under ultrasound guidance. The FNA is sent to the pathologist and results generally take less than one week. These biopsy results are generally reported on a Bethesda rating scale of one to six and will require your physician to interpret those results for you. Ninety percent of biopsies are benign. Benign nodules should undergo serial ultrasounds every 6-12 months, because although FNA is highly accurate, it is not 100% in making a diagnosis. If nodules are observed to enlarge over time, then surgery is recommended to rule out cancer. For biopsies that show suspicion of cancer, surgery is recommended immediately. There are some types of thyroid nodules (follicular tumors) where FNA cannot distinguish benign from malignant nodules. These nodules in the past have been managed by surgery but can now be sent for genetic testing from the FNA sample to determine if surgery can be safely avoided.
Thyroid operations can be divided into several categories, including a lobectomy which is a one-sided removal of the thyroid gland, total thyroidectomy, removal of both sides of the thyroid gland, or subtotal thyroidectomy, variations in which all of one side the gland and part of the other side of the gland are removed. Many patients are able to go home the same day after surgery, avoiding an overnight hospital stay which reduces the risk of infection and blood clots as well as lower medical bills for the patient.
The thyroid is surgically removed through a horizontal incision on the neck approximately two inches long. The incision is closed with dissolving stitches that are underneath the skin and are not visible and will not need removal. The stitches typically take a few months to dissolve. Until the first postop appointment in one week, the incision is covered with steri-strips (tape). The steri-strips will be removed for you in our office in one week with the use of an adhesive remover solution. You do not need to do anything to the incision for the first week. You may shower and get the incision wet 24 hours after your surgery. Once the steri-strips have been removed (a week after surgery), use of Mederma® Scar Cream Plus SPF 30 is recommended twice a day for 2 months for better cosmetic results.
Some difficulty swallowing is expected after surgery. You may advance your diet from liquids to soft foods and then to regular food as the swelling gradually improves over the first week.
You should avoid strenuous exertion such as heavy lifting or cardio exercise for the first two weeks after surgery. Activities that don’t involve heavy lifting or increasing the heart rate such as walking are not only safe, but recommended. It is common to feel less energy for a few weeks after surgery that gradually improves.
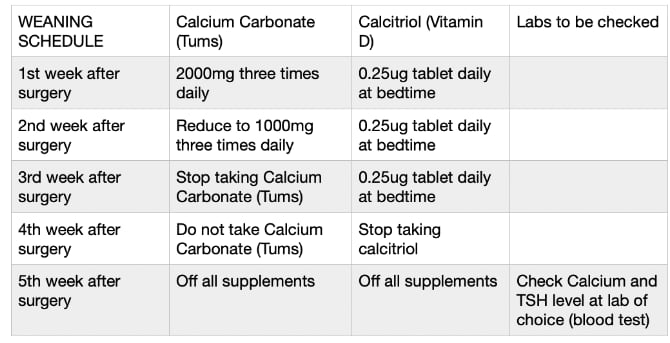
You may take over the counter ibuprofen after surgery for pain. You may take one to three tablets every 4-6 hours as needed for pain with food to reduce the risk of stomach irritation and ulcer. You will also be prescribed a narcotic pain medication that can be taken along with the ibuprofen if needed. Common side effects of all narcotics include drowsiness, nausea, and constipation. If you have had a total thyroidectomy, you will also be prescribed levothyroxine (thyroid hormone replacement) to be taken once daily to be taken indefinitely. Patients often have significant drop in their blood calcium levels after total thyroidectomy due to manipulating or “bruising” of the parathyroid glands. You will also be prescribed calcium carbonate which is Tums, 2000mg three times daily as well as calcitriol (Vitamin D) 0.25mcg to be taken once daily at bedtime. These should be started immediately after surgery. It is beneficial to take the calcitriol once daily at bedtime to prevent low calcium levels through the night.
After your first postop appointment, you will likely be instructed to wean off the calcium and calcitriol supplements if you have not experienced symptoms of low calcium. The typical weaning schedule starting after the one week postop appointment is in the chart below:
There are three conditions that must be met in order to resume driving after surgery. You must wait at least 24 hours after receiving general anesthesia to drive. In addition, you must be able to turn your neck well to look for traffic. Lastly, you cannot drive while taking narcotics for pain.
Many patients notice a subtle change in their voice quality for the first few weeks postoperatively. Although trauma to the nerves supplying the vocal cords on one or both sides of the voice box may occur during thyroidectomy, frank hoarseness or trouble swallowing is a rare complication. If you have any questions regarding the fact that your voice may be excessively hoarse or raspy, or if you are experiencing any type of coughing or choking when you attempt to swallow, please call our office.
A potentially serious or life-threatening complication of thyroidectomy, which can occur rather abruptly, is formation of a hematoma due to bleeding. If you feel that there has been an abrupt swelling or outward displacement of the wound area in the lower neck, or if the neck wound suddenly starts exhibiting more tenderness, redness, bruising or bogginess than you would expect, you need to contact our office immediately. If you feel any shortness of breath, you should proceed to the emergency room as quickly as possible.
For patient undergoing a total or subtotal thyroidectomy, low blood calcium levels after surgery can occur due to manipulating or “bruising” of the parathyroid glands. The symptoms of low calcium would include tingling around the mouth or in the hands or feet, generalized weakness, muscle cramps or feelings of the heart exhibiting an abnormal rate or irregular beat. If any of these symptoms occur, please take extra doses of Tums and call our office immediately.
Calcium and narcotics often cause constipation so use of over the counter Colace or Miralax can be helpful to prevent that problem.
It is common to have swelling of the neck after surgery that is gradually improving, but please call our office if you notice redness, swelling, or discharge from the incision that is worsening rather than improving with time. Occasionally, the body will reject the dissolving stitches in the first few months after surgery. If you notice redness, swelling or discharge from the incision, call our office.
Contact phone number: (815) 725-1191 office/24 hour answering service.
 Parathyroidectomy
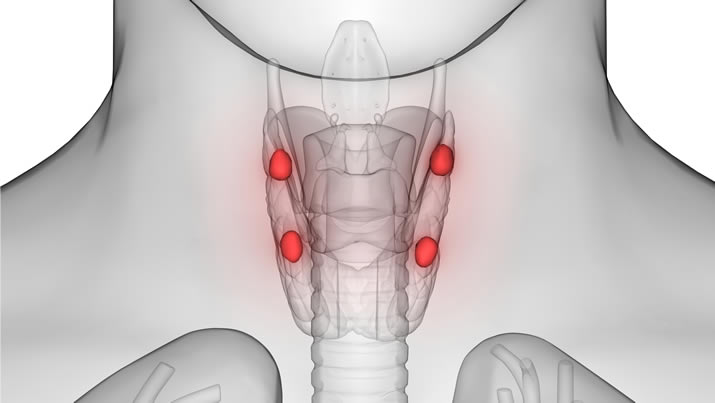
ParathyroidectomyGenerally, the body has four parathyroid glands that are normally the size of a grain of rice, two on each side of the neck usually hugging the thyroid gland. The parathyroid glands act like thermostats to keep the calcium level in the blood at the normal level (normal calcium is 8.5-10). Occasionally, one or more of the parathyroid glands become overactive and enlarged causing the blood calcium to be high similar to a bad thermostat. So then the overactive parathyroid gland (defective thermostat) needs to be removed to prevent calcium from being pulled out of the bones (osteoporosis) and spilled into the urine (kidney stones). This is called parathyroidectomy. This requires an experienced surgeon because the parathyroid glands are sometimes not where they are supposed to be (ectopic locations). Sometimes more than one parathyroid gland is overactive (15%) and this requires removing 2 or more parathyroid glands. We draw blood tests for PTH levels during surgery to make sure the surgery is successful. If the overactive parathyroid gland has been correctly removed, then the blood PTH level should drop within 30 minutes during surgery. In this particular video, the patient had a rare condition called parathyroid hyperplasia (3%) where all 4 parathyroid glands are enlarged. In this case, three and a half parathyroid glands were removed. Half a gland is left to prevent the calcium from falling too low.
Please call one of our locations: West Joliet 815-725-1191, New Lenox 815-717-8768, and Morris 815-941-1972 to schedule an appointment.
Contact Us Today!