Chicagoland’s premier Sleep and Snoring Center. ENT Surgical Consultants is proud to serve our patients with outstanding, comprehensive, cutting edge, and state-of-the-art diagnostic Sleep and Snoring Care. Please contact us today for a consultation 815-725-1191.
Forty-five percent of normal adults snore at least occasionally, and 25 percent are habitual snorers. Problem snoring is more frequent in males and overweight persons, and it usually grows worse with age. Snoring is an indication of obstructed breathing. Therefore, it should not be taken lightly. An otolaryngologist can help you to determine where the encumbrance may be and offer solutions for this noisy and often embarrassing behavior.
The noisy sounds of snoring occur when there is an obstruction to the free flow of air through the passages at the back of the mouth and nose. This area is the collapsible part of the airway (see illustration) where the tongue and upper throat meet the soft palate and uvula. Snoring occurs when these structures strike each other and vibrate during breathing.
In children, snoring may be a sign of problems with the tonsils and adenoids. A chronically snoring child should be examined by an otolaryngologist, as a tonsillectomy and adenoidectomy may be required to return the child to full health.
Also, deformities of the nose or nasal septum, such as a deviated septum (a deformity of the wall that separates one nostril from the other) can cause such an obstruction.
Socially – It can make the snorer an object of ridicule and causes others sleepless nights and resentfulness.
Medically – It disturbs sleeping patterns and deprives the snorer of appropriate rest. When snoring is severe, it can cause serious, long-term health problems, including obstructive sleep apnea.
When loud snoring is interrupted by frequent episodes of totally obstructed breathing, it is known as obstructive sleep apnea. Serious episodes last more than ten seconds each and occur more than seven times per hour. Apnea patients may experience 30 to 300 such events per night. These episodes can reduce blood oxygen levels, causing the heart to pump harder.
The immediate effect of sleep apnea is that the snorer must sleep lightly and keep his muscles tense in order to keep airflow to the lungs. Because the snorer does not get a good rest, he may be sleepy during the day, which impairs job performance and makes him a hazardous driver or equipment operator. After many years with this disorder, elevated blood pressure and heart enlargement may occur.
Heavy snorers, those who snore in any position or are disruptive to the family, should seek medical advice to ensure that sleep apnea is not a problem. An otolaryngologist will provide a thorough examination of the nose, mouth, throat, palate, and neck. A sleep study in a laboratory environment may be necessary to determine how serious the snoring is and what effects it has on the snorer’s health.
Treatment depends on the diagnosis. An examination will reveal if the snoring is caused by nasal allergy, infection, deformity, or tonsils and adenoids.
Snoring or obstructive sleep apnea may respond to various treatments now offered by many otolaryngologist—head and neck surgeons:
If surgery is too risky or unwanted, the patient may sleep every night with a nasal mask that delivers air pressure into the throat; this is called continuous positive airway pressure or “CPAP”.
More than 300 devices are registered in the U.S. Patent and Trademark Office as cures for snoring. Some are variations on the old idea of sewing a sock that holds a tennis ball on the pajama back to force the snorer to sleep on his side since snoring is often worse when a person sleeps on his back. Some devices reposition the lower jaw forward; some open nasal air passages; a few others have been designed to condition a person not to snore by producing unpleasant stimuli when snoring occurs. But, if you snore, the truth is that it is not under your control. If anti-snoring devices work, it is probably because they keep you awake.
Adults who suffer from mild or occasional snoring should try the following self-help remedies:
Sleep apnea is a common disorder that can be serious. In sleep apnea, your breathing stops or gets very shallow. Each pause in breathing typically lasts 10 to 20 seconds or more. These pauses can occur 20 to 30 times or more an hour.
The most common type is obstructive sleep apnea. That means you are unable to get enough air through your mouth and nose into your lungs. When that happens, the amount of oxygen in your blood may drop. Normal breaths resume with a snort or choking sound. People with sleep apnea often snore loudly. However, not everyone who snores has sleep apnea.
When your sleep is interrupted throughout the night, you can be drowsy during the day. People with sleep apnea are at higher risk for car crashes, work-related accidents and other medical problems. If you have it, it is important to get treatment.
Excessive body weight contributes to snoring and obstructive sleep apnea, in addition to being a major influence on general health and well-being. Obstructive sleep apnea occurs in about 50-60% of those who are obese. A recent report from the National Center for Health Statistics concludes that seven of 10 adults don’t regularly exercise, and nearly four in 10 aren’t physically active. Lack of exercise can increase the risk of diabetes, heart disease, and stroke. About 300,000 people in the U.S. die each year from diseases related to inactivity. Proper diet and exercise are the mainstays for a healthy lifestyle, although many Americans turn to costly fad diets and exercise programs that fail to provide weight loss and a healthy lifestyle. The basic tenets to gradual weight loss and good health include developing healthy eating habits and increasing daily physical activity.
Self-help guidelines for healthy activity:
Make your activity enjoyable – listen to music, include family and friends, etc.
For those who are already regularly moderately active, increase the duration and intensity for additional benefits.
Weight loss tips:
The healthy weight approach to dieting:
Restless Legs Syndrome
People with this disorder have "crawling" sensations in their sleep. The sensation goes away as soon as they get up to "walk it off". Good sleep hygiene, exercise, and avoiding caffeine and other stimulants may help.
Periodic Limb Movement Disorder
Some people's legs or arms jerk repeatedly during sleep. In the morning, they awake feeling tired. This disorder can be diagnosed in the sleep center. Medications (Sinemet, etc.) may help in some cases.
Insomnia
Trouble falling or staying asleep which disrupts your daily life. There are many causes that require specific treatment, but good sleep hygiene often helps.
Narcolepsy
Falling asleep unexpectedly many times a day. This can be embarrassing and dangerous. Good sleep hygiene, medications, and scheduled naps are beneficial.
Will my insurance provider pay AIRLIFT Hyoid and Tongue suspension procedures?
Most insurance providers including Medicare and Medicaid will pay for Hyoid Suspension procedures, provided you have undergone a sleep study (Polysomnography) and at least tried CPAP long enough to prove that you will not or cannot tolerate the device. Private insurance does not commonly pay for Tongue Suspension procedures.
Q: What can I expect immediately after surgery?
Patients may experience approximately 5-7 days of difficulty swallowing and/or talking after AIRLIFT Tongue suspension procedure, along with mild to moderate pain. Patients who undergo the AIRLIFT Hyoid Suspension procedure may experience increased effort to swallow for 1-2 weeks and swelling at the surgical site that may last up to 1 month.
Do most people get the AIRLIFT procedures at the same time as palate surgery?
Yes, most AIRLIFT surgeries are performed in conjunction with other procedures such as UPPP, pillars or nasal surgery, due to the fact that the majority of sleep apneics suffer from multi-point, multi-level obstruction (i.e. tongue, lower airway, palate and nose). On the other hand, a significant number of surgeons opt to stage surgery to limit the number of procedures you undergo at one sitting, based on their individual assessment of your primary point(s) of obstruction. In other words, your surgeon may perform a AIRLIFT Hyoid Suspension as your initial surgery. After a follow-up sleep study, if you still suffer from sleep apnea, your surgeon will then schedule you for a second surgery (UPPP or similar) designed to address your airway narrowing near your tonsils and soft palate.
I have been diagnosed with both hypertension and sleep apnea. Are they related in any way?
Yes, hypertension is frequently the result of sleep apnea. Depression, daytime sleepiness and sometimes congestive heart failure may all be associated with OSA. In children, sleep apnea has been found to lead to or be the cause of Attention Deficit Disorder.
The doctor who conducted my sleep study told me surgery does not work. Is this true?
While there is little dispute that CPAP is approximately 95% effective in curing OSA, patient compliance clocks in at a dismal 40-45%. In short, there has been some historic misunderstandings from both the sleep lab physician and the practicing sleep surgeon. Now, with the advent of quick, minimally invasive surgeries such as the Repose procedures, surgeons can now achieve cures rates in the range of 75-90% when performed in conjunction with palate and nasal surgery. In light of the low compliance numbers associated with CPAP use, Repose surgery in conjunction with palate surgery may very well achieve results far greater than that of mechanical, external CPAP.
 or Sleep Apnea Surgery
or Sleep Apnea SurgeryThe tonsils play an important role as a defense system against infections in the upper respiratory tract during childhood. The tonsils are lymphoid tissues located in the back and on each side of the throat. The adenoid tonsil is also made up of lymphoid tissue and is located in the upper back part of the throat behind the nose. They work together to “catch” and trap incoming infections. Unfortunately, the tonsil and adenoid may become the source of infection itself like a plugged filter or block the upper airway.
Tonsillectomy is recommended for adults with signs and symptoms of:
Numerous medical studies have definitively proven that removal of the tonsils is helpful for the above problems without resulting in any long-term negative impact on the immune system. Fortunately, there is ample other lymphoid tissue still remaining in the throat to perform its immune function (i.e., lingual tonsils on the back of the tongue, accessory tonsils on the back wall of the throat, Gerlach tonsils near the Eustachian tube opening, etc).
Sleep apnea surgery may be performed simultaneously. Surgery most commonly involves shortening the soft palate and uvula at the same time as tonsillectomy. This procedure tightens the loose tissue in the throat to relieve the obstruction of the upper throat. This is called uvulopharyngopalatoplasty or more simply UPPP.
If your obstruction includes the lower throat, your doctor may also perform a procedure called geniohyoid advancement (GHA) with thyrohyopexy (THP). The purpose of this procedure is to pull the back of the tongue forward to increase the size of the lower throat. This procedure requires additional incisions on the inside of the mouth behind the lower lip and also in the front of the upper neck.
The throat heals so well after surgery because of its excellent blood supply. Unfortunately, this is the major reason that the most common major complication after tonsil and adenoid removal is hemorrhage, or excessive bleeding. This occurs in 4% of patients and most commonly occurs six to twelve days following surgery. It is extremely important to notify your doctor before surgery if you or anyone in your family has a tendency to bleed or hemophilia. This includes frequent nosebleeds, easy bruising, excessive bleeding with previous tonsil, dental or other surgery, abnormally heavy menstrual periods, prolonged bleeding after cuts or scrapes, and previous blood transfusions.
The following complications have been known to rarely occur:
Download (UPPP) Pre and Post Operative Surgery Instructions
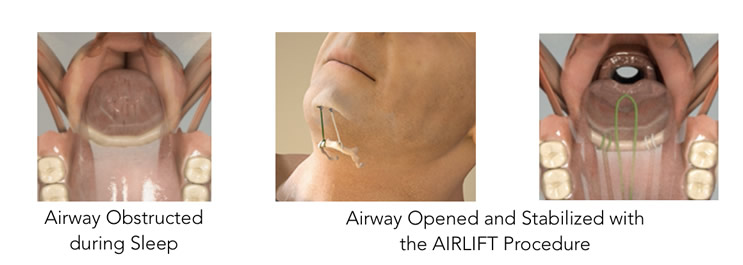
The AIRLIFT® Hyoid and Tongue suspension procedures are simple and effective surgical treatments for sleep apnea (OSA). In the AIRLIFT procedure, small implants are placed behind the chin and sutures are looped around the hyoid bone or into the base of the tongue. The sutures are tightened, which pulls the hyoid bone and/or tongue base forward which opens and enlarges the airway and then attached to the implants to keep tension. The AIRLIFT procedures are and intuitive approach to hyoid & tongue suspension designed to provide immediate and lasting relief by opening and stabilizing the airway. AIRLIFT is easy to implant, comfortable and covered by insurance. Find more information at www.siestamedical.com

Coblation® Soft Palate Treatment can reduce the incidence of snoring without the discomfort and inconvenience associated with traditional surgery. Coblation Soft Palate Treatment is performed with the ReFlex Ultra® 55 Wand and can be performed in an outpatient setting under local anesthesia. The procedure typically takes less than fifteen minutes and the patient will experience a reduction in snoring within six weeks.
In addition, studies published in peer-reviewed journals have shown Coblation Soft Palate Treatment to have numerous clinical advantages:
 Now there's a simple, safe, minimally invasive treatment for snoring and mild to moderate obstructive sleep apnea (OSA). Unlike other painful and invasive surgical procedures, the Pillar Procedure is a simple treatment that your doctor can perform in a single short office visit or in combination with other procedures. More than 30,000 people worldwide have been treated with the Pillar Procedure.
Now there's a simple, safe, minimally invasive treatment for snoring and mild to moderate obstructive sleep apnea (OSA). Unlike other painful and invasive surgical procedures, the Pillar Procedure is a simple treatment that your doctor can perform in a single short office visit or in combination with other procedures. More than 30,000 people worldwide have been treated with the Pillar Procedure.
During the Pillar Procedure, three tiny polyester implants are placed into the soft palate. Over time, the implants, together with the body's natural fibrotic response, add structural support to and stiffen the soft palate. This structural support and stiffening reduce the tissue vibration that can cause snoring and the palatal tissue collapse that can obstruct the upper airway and cause obstructive sleep apnea (OSA).
Clinical studies of the Pillar Procedure have shown that:
This informative 3D animation provides a simple, visual explanation of the causes of palatal OSA and snoring. The video makes it easy to see how the placement of three tiny implants helps correct the palatal vibration and collapse that can cause snoring and obstructive sleep apnea. The Pillar Procedure targets the most common cause of snoring and obstructive sleep apnea (OSA)—the soft palate.1,2 During the Pillar Procedure, three tiny woven implants are placed in the soft palate. Over time the implants, together with the body's natural fibrotic response, add structural support to and stiffen the soft palate. This structural support and stiffening reduce the tissue vibration that can cause snoring and the palatal tissue collapse that can obstruct the upper airway and cause obstructive sleep apnea (OSA). Pillar implants are made of a material that has been used in implantable medical devices for more than 50 years. Patients cannot see or feel the Pillar implants, nor do they interfere with swallowing or speech. Many patients resume normal diet and activities the same day of the procedure.