
Chicagoland’s premier voice and swallowing specialists. ENT Surgical Consultants is proud to serve our patients with outstanding, comprehensive, cutting edge, and state-of-the-art diagnostic Voice and Swallowing Care. Please contact us today for a consultation 815-725-1191.
Vocal cord paralysis is a voice disorder that occurs when one or both of the vocal cords (or vocal folds) do not open or close properly. Vocal cord paralysis is a common disorder, and symptoms can range from mild to life threatening.
The vocal cords are two elastic bands of muscle tissue located in the larynx (voice box) directly above the trachea (windpipe). The vocal cords produce voice when air held in the lungs is released and passed through the closed vocal cords, causing them to vibrate. When a person is not speaking, the vocal cords remain apart to allow the person to breathe.
Someone who has vocal cord paralysis often has difficulty swallowing and coughing because food or liquids slip into the trachea and lungs. This happens because the paralyzed cord or cords remain open, leaving the airway passage and the lungs unprotected.
What causes vocal cord paralysis?
Vocal cord paralysis may be caused by head trauma, a neurologic insult such as a stroke, a neck injury, lung or thyroid cancer, a tumor pressing on a nerve, or a viral infection. In older people, vocal cord paralysis is a common problem affecting voice production. People with certain neurologic conditions, such as multiple sclerosis or Parkinson's disease, or people who have had a stroke may experience vocal cord paralysis. In many cases, however, the cause is unknown.
People who have vocal cord paralysis experience abnormal voice changes, changes in voice quality, and discomfort from vocal straining. For example, if only one vocal cord is damaged, the voice is usually hoarse or breathy. Changes in voice quality, such as loss of volume or pitch, may also be noticeable. Damage to both vocal cords, although rare, usually causes people to have difficulty breathing because the air passage to the trachea is blocked.
People who have vocal cord paralysis experience abnormal voice changes, changes in voice quality, and discomfort from vocal straining. For example, if only one vocal cord is damaged, the voice is usually hoarse or breathy. Changes in voice quality, such as loss of volume or pitch, may also be noticeable. Damage to both vocal cords, although rare, usually causes people to have difficulty breathing because the air passage to the trachea is blocked.
Vocal cord paralysis is usually diagnosed by an otolaryngologist. A doctor who specializes in ear, nose, and throat disorders. Noting the symptoms the patient has experienced, the otolaryngologist will ask how and when the voice problems started in order to help determine their cause. Next, the otolaryngologist listens carefully to the patient's voice to identify breathiness or harshness. Then, using an endoscope--a tube with a light at the end--the otolaryngologist looks directly into the throat at the vocal cords. A speech-language pathologist may also use an acoustic spectrograph, an instrument that measures voice frequency and clarity, to study the patient's voice and document its strengths and weaknesses.
There are several methods for treating vocal cord paralysis, among them surgery and voice therapy. In some cases, the voice returns without treatment during the first six months after damage. For that reason, doctors often delay permanent corrective surgery for at least six months to be sure the voice does not recover spontaneously. During this time, the suggested treatment is usually voice therapy and sometimes injecting the vocal cord with temporary bulking agents. Speech therapy may involve exercises to strengthen the vocal cords or improve breath control during speech.
Surgery involves injecting bulk to the paralyzed vocal cord or changing its position. To add bulk, an otolaryngologist injects a substance, commonly Teflon, into the paralyzed cord. This is done with a needle and syringe and does not require an incision. Other substances currently used are collagen, a structural protein; silicone, a synthetic material; and body fat. The added bulk reduces the space between the vocal cords so the nonparalyzed cord can make closer contact with the paralyzed cord and thus improve the voice. RADIESSE Voice is an injectable implant containing synthetic Calcium Hydroxylapatite (CaHA) microspheres, which have a diameter range of 25 to 45 µm, suspended in an aqueous gel carrier. These consistently shaped and sized particles have proven safe and biocompatible while allowing gradual tissue in growth for a long lasting augmentation shown to be effective up to 12-24 months.
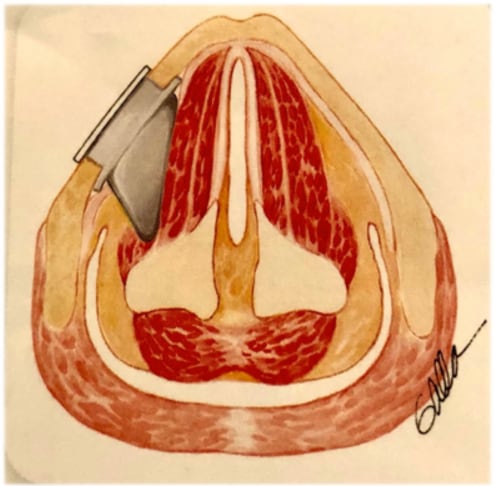
Sometimes an operation (Medialization Laryngoplasty also called Thyroplasty) that permanently shifts a paralyzed cord closer to the center of the airway to improve voice and swallowing. This is done with a permanent implant through an incision in the neck using and implant such as the Montgomery® Thyroplasty Implant System.
Treating people who have two paralyzed vocal cords may involve performing a surgical procedure called a tracheotomy to help breathing. In a tracheotomy, an incision is made in the front of the patient's neck and a breathing tube (tracheotomy tube) is inserted through a hole, called a stoma, into the trachea. A Passy Muir® Valve placed onto the tracheostomy tube allows the patient to still be able to talk.
RADIESSE Voice Gel is an injectable implant containing synthetically derived polymers, and no CaHA microspheres, suitable for 1-2 month, short-term vocal fold augmentation, in patients where reversible nerve damage is suspected, or in patients wishing a short term augmentation before making a decision to have a long term augmentation done with RADIESSE Voice.
The injection volume and location should conform to the following recommendations:
The gel carrier dissipates over a few months allowing for new tissue infiltration. The CaHA particles gradually break down and are metabolized over several years into calcium and phosphate ions through the body’s own normal metabolic processes. In treatment of vocal fold insufficiency, RADIESSE Voice should provide a correction that lasts 1-2 years. RADIESSE® Voice Gel provides short-term improvement for 1-2 months.
There are few reported side effects and those reported are commonly associated with injection of implant materials. These may include pain and tenderness at the injection site.
No, RADIESSE Voice will remain soft and pliable.
 Medialization Laryngoplasty/Thyroplasty
Medialization Laryngoplasty/ThyroplastyThis operation allows the nonparalyzed cord to make better contact with the paralyzed cord. Shifting the position of the paralyzed vocal cord towards the opposite moving vocal cord improves both voice and swallowing. This requires a small incision in the neck to place a silastic or gortex implant in to the voice box (thyroid cartilage) to permanently move the paralyzed vocal cord towards the midline to better align with the opposite moving vocal cord. Towards the top of the page is a video of a patient who underwent such a procedure using the Montgomery Thyroplasty Implant System.
After these operations, patients may also undergo voice therapy, can help fine-tune the voice.
A tracheostomy is a surgical procedure to create an opening through the neck into the trachea (windpipe). A tube is usually placed through this opening to provide an airway and to remove secretions from the lungs. This tube is called a tracheostomy tube or trach tube.
A tracheostomy may be done if you have:
If the tracheostomy is temporary, the tube will eventually be removed. Healing will occur quickly, leaving a minimal scar.
Occasionally a stricture, or tightening, of the trachea may develop, which may affect breathing.
If the tracheostomy tube is permanent, the hole remains open and may require surgical closure when no longer needed.
Most patients require 1 to 3 days to adapt to breathing through a tracheostomy tube. It will take some time to learn how to communicate with others. Initially, it may be impossible for the patient to talk or make sounds.
After training and practice, most patients can learn to talk with a tracheostomy tube. Patients or family members learn how to take care of the tracheostomy during the hospital stay. Home-care service may also be available.
Normal lifestyles are encouraged and most activities can be resumed. When outside, a loose covering (a scarf or other protection) for the tracheostomy stoma (hole) is recommended. Patients must adhere to other safety precautions regarding exposure to water, aerosols, powder, or food particles as well.
A Passy Muir Valve placed onto the tracheostomy tube allows the patient to still be able to talk.

Laryngectomy is surgery to remove the larynx (voice box) in your throat. All or part of the larynx may be removed in a laryngectomy.
Total laryngectomy is major surgery that is done in the hospital. Before surgery you will receive general anesthesia. This will make you unconscious and unable to feel pain.
In a total laryngectomy, first your surgeon will make an incision (cut) in your neck to open up the area. Important parts of this surgery are:
Part of your pharynx may be removed in a total laryngectomy. Your pharynx is the tube air moves through from your nose. It connects with your larynx. The surgery takes 5 to 9 hours.
Usually laryngectomy is done to treat cancer of the larynx. It is also done to treat:
You will have many doctor visits and medical tests before you have surgery. Some of these are:
Always tell your doctor or nurse:
During the days before your surgery:
On the day of your surgery:
You will need to stay in the hospital for several days after surgery.
After the procedure, you will be groggy and will not be able to speak. An oxygen mask will be on your stoma. It’s important to keep your head raised, rest a lot, and move your legs from time to time to improve blood flow. Keeping blood moving reduces your risk of getting a blood clot.
You can use warm compresses to reduce pain around your incision. Your nurse will give you pain medicine.
You will receive nutrition through an IV (a tube that goes into a vein) and tube feedings. Tube feedings are given through a tube that goes through your stoma and into your esophagus (swallowing tube).
You may be allowed to swallow food as soon as 2 to 3 days after surgery. But, it is more common to wait 5 to 7 days after your surgery to start eating through your mouth.
Your trachea drain will be removed in 2 to 3 days. You will be taught how to care for your tracheostomy tube and stoma. You will learn how to safely shower or swim. You must be careful not to let water enter through your stoma.
Speech rehabilitation with a speech therapist will help you relearn how to speak.
You will need to avoid heavy lifting or strenuous activity for about 6 weeks. You may slowly resume your normal, light activities.
Follow up with your doctor as often as your doctor says you need to.
Your wounds will take about 2 to 3 weeks to heal. You can expect full recovery in about a month. Many times, removal of the larynx will take out all the cancer or injured material. People learn how to change their lifestyle and live without their voice box.